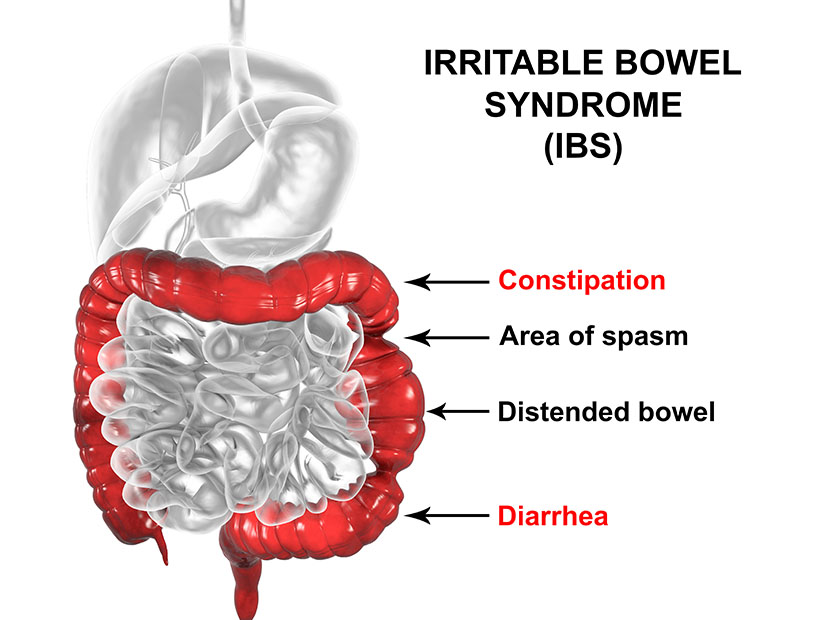
Coral Springs, Florida – Irritable bowel syndrome (IBS) is a well-known gastrointestinal disorder. It is characterized by a group of symptoms with no known pathogen. Typical symptoms include abdominal cramps with bloating and excessive gas, diarrhea alternating with constipation, the abdominal pain triggered by eating and relieved after a bowel movement. In most cases, mucus is present in the stool. Other symptoms may include emotional disturbances, anxiety, headache, chronic fatigue, poor appetite and fibromyalgia. IBS accounts for more than 50% of outpatient referrals for GI specialists, and it is estimated that one out of three adults suffers from IBS in United States. In addition, women have a higher rate of IBS than men.
What causes IBS?
Doctors aren’t sure what causes IBS. Experts think that a combination of problems may lead to IBS. The following factors may contribute to IBS:
- Disrupted peristalsis. Peristalsis is the natural rhythm and movement of the GI tract. When the smooth muscles inside the intestines are out of rhythm, food is eliminated from the intestines too soon (diarrhea) or too slowly (constipation).
- Low levels of microflora, the good bacteria in the intestinal tract. The human body needs good bacteria to ferment food. When the flora level is low, nutrients cannot be absorbed, and wastes build up; the end result is bloating and abnormal bowel movements.
- Sugar sensitivity. Studies show foods such as some carbohydrates that contain high FODMAPS (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) often contribute to many IBS symptoms.
- Emotional disturbance. Stress can cause serotonin imbalance in the gut, interrupting the normal function of brain-gut network.
- Small intestinal bacterial or candida overgrowth, and other food intolerances or sensitivities are also contributors to IBS.
Diagnosis and Treatment of IBS in Conventional Medicine
By definition in Western medical theory, a functional disorder is one where there is no known structural, biochemical or infectious cause. There is no one, specific test for IBS. As mentioned previously, IBS is a group of complex disorders, based on clinical symptoms. To help doctors confirm IBS, they are likely order the following tests: stool study, colonoscopy, endoscopy, gluten and lactose intolerance tests, and even an abdominal CT scan. Once other life-threatening conditions are ruled out, a diagnosis of IBS can be made.
Treatments for IBS mostly focus on relieving symptoms and restoring function. Common treatments are lifestyle changes and psychotherapy. In some cases, medications including colon relaxers, anti-diarrheals, antibiotics and anti-anxiety medications may be prescribed. Unfortunately, many people experience side effects from any or all these types of pharmaceutical interventions.
Traditional Chinese Medicine (TCM) Theory and IBS
Chinese medical literature is unanimous in saying that the root cause of IBS is always a disharmony between the liver and spleen. IBS is commonly associated with Liver Qi stagnation overacting on the spleen and stomach system (digestion). In TCM, the Liver is responsible for the smooth movement of Qi (energy), blood, and body fluids throughout the body. The TCM “liver” matches autonomic nervous system in Western medicine which responds to stress, including the bodily functions such as peristalsis and bowel movements over which we have no control. Liver acts as a traffic control police officer that directs the flow of Qi.
The Spleen, on other hand, is in charge of transformation and transportation functions, extracting the essence (nutrients) from food and transforming liquids; it is the core energy source for sustaining the physical needs. The disharmony of the Liver and Spleen can therefore lead to constipation, diarrhea, or a combination of both, along with pain and bloating, which are the major presentations of IBS. Etiologies include:
Emotional stress is the most common factor inducing IBS. Anger, frustration, and emotional suppression hinder the Liver‘s function to ensure smooth flow of the Qi. Liver Qi stagnation results in abdominal distention and pain.
Improper diet directly impairs the stomach and spleen system’s function to help absorb the nutrients from food. Over-consuming greasy and sweet foods results in food retention and “damp heat”; eating cold and raw food directly injures the spleen and stomach and produces damp cold. Both lead to abnormal bowel movements, including diarrhea and constipation.
Weak spleen and stomach is pre-existing factor of individuals who are more susceptible to exterior pathogens. Long-term use of antibiotics also injure the Spleen Qi, resulting in fatigue and diarrhea.
TCM Treatments for IBS
Traditional Chinese Medicine has long history of treating IBS. Evidence-based medicine has demonstrated that irritable bowel syndrome (IBS) can improve with multiple treatment options addressing this often complex disorder. One of these options is Traditional Chinese Medicine (TCM), including acupuncture, herbal formulas, and dietary therapy.
Acupuncture has been used to treat several gastrointestinal symptoms including IBS in China for centuries. Acupuncture can regulate organ system function, gastric emptying, and acid secretion by altering neurotransmitter systems. Studies have shown that the application of acupuncture targeting serotonergic, cholinergic and glutamatergic pathways in IBS patients can increase the concentration of endogenous opioids, which then reduces organ and pain perception.
A recent research study confirms that acupuncture significantly reduces abdominal pain and diarrhea, and promotes normal stools. When this study was conducted on IBS patients, it showed the effective rate was 96.7% with many patients experiencing a complete recovery without relapses, and over 65% of patients’ IBS had “significantly improved.” As a standalone procedure, acupuncture demonstrated a 76.7% total effective rate including reductions in abdominal pain, diarrhea, and frequency of bowel movements.
TCM represents one aspect of the Chinese medical philosophy, which is characterized by its emphasis on maintaining and restoring balance in the human body. Herbal medicine is usually prescribed alongside acupuncture for IBS to achieve optimal health. In a 2015, a review of Chinese herbal formulas and IBS, patients taking traditional Chinese herbs alone or in conjunction with acupuncture improved at a higher percentage than those using only conventional medicine. The authors pointed out that Chinese herbal formulas demonstrate healing effects which include strengthening the rhythm of smooth muscle of the gastrointestinal tract, regulating the level of serotonin, and reducing intestinal inflammation.
One of the famous herbal formulas to treat IBS is Tong Xie Yao Fang (Essential Formula for Painful Diarrhea). This formula is composed of four simple herbs: Bai Shao (white peony), Bai Zhu (white atractylodes), Chen Pi (citrus peel) and Fang Feng (siler). Bai Zhu fortifies the spleen, dries dampness and treats Spleen vacuity; in other words, it helps the absorption of the nutrients of the small intestine. Bai Shao nourishes the blood, courses the Liver, and reduces Liver dominance to relieve stress. Together, these two harmonize the Liver and Spleen, supplementing the Spleen and draining the Liver. Chen Pi helps the Qi flow in the proper direction, dries dampness, and it supports the digestive function by reducing abdominal bloating. Fang Feng correct the Qi direction of the liver and intestines, and stops the painful diarrhea.
This formula can be modified for individuals based on the differentiation of symptoms according to traditional Chinese medicine diagnostic patterns. For example, in the case of dry stool, Ma Zi Ren Wan can be added to the previous formula. For prolonged diarrhea causing poor appetite, it is more effective to combine this formula with Shen Ling Bai Zhu San to strengthen the spleen. Hence, using Chinese herbal medicine is a strategy that provides the patient with individualized and comprehensive treatments to correct the underlying issue along with the symptoms. All the above herbal formulas are available in pill or tablet form for patients’ convenience as well as powders to make into teas.
Lifestyle Recommendations
TCM and Western medicine agree that IBS can improve with some lifestyle or diet choices. Some of them are:
- Avoiding cold or raw foods, spicy or greasy foods, and sugar in the diet. Cold foods tax and weaken digestion because the body has to work to “cook” the food before it can be digested. Greasy or spicy foods add heat to the digestive system and can trigger diarrhea or burning sensations in the esophagus or during defecation. Also, sugar and some carbohydrates that have FODMAPs can worsen gas and bloating symptoms.
- Avoid “intolerance” foods such as gluten and milk products. Many people with IBS are sensitive to these foods, even if they are not “allergic” or have celiac disease, and their symptoms improve while avoiding them.
- Get plenty of rest and moderate exercise. These work together to reduce stress and improve digestion and circulation.
Conclusion
IBS is a complex set of symptoms that is treatable with acupuncture, herbs, and lifestyle choices. TCM can treat the underlying stress in the body, strengthening digestion, and balancing the body can relieve not only the symptoms of IBS but help the patient achieve wellness. Schedule a consultation with one of our acupuncturists today at our Coral Springs / Margate, Florida wellness center.
References
- 中医内科学。中国中医药出版社。2007 年第二版。
- 黄帝内经。 中华书局。2010 年。
- Anshen Shi. Internal Medicine. Bridge Publishing Group. 2003.
- Bob Flaws and Philippe Sionneau. The Treatment of Modern Western Medical Diseases with Chinese Medicine. Blue Poppy Press, 2018.
- Huang, Kee Chang. The Pharmacology of Chinese Herbs. CRC Press, 1999
- “IBS Treatment.” Acupuncture Melbourne | Best Acupuncture & Chinese Medicine Melbourne. Web. <http://evergreencmc.com.au/irritable-bowel-syndrome-ibs/>.
- “Irritable Bowel Syndrome (IBS).” The Traditional Chinese Approach to Digestive Problems – Fusion Health, Fusion Health, 2017, www.fusionhealth.com.au/health-categories/digestion-liver-detox/irritable-bowel-syndrome-ibs.
- “Irritable bowel syndrome – Symptoms and causes – Mayo Clinic.” Mayo Clinic – Mayo Clinic. Web. <http://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016>.
- “Symptoms & Causes of Irritable Bowel Syndrome | NIDDK.” National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Web. <http://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome/symptoms-causes>.
- “Traditional Chinese Medicine and IBS.” Integrative Medicine Doctors, Acupuncture, Massage, Naturopathic, Nutritional Counseling, Primary Care Albany NY Upstate New York. Web. <http://stramcenter.com/blog/blog-detail/traditional-chinese-medicine-and-ibs/>.
- “Treatment of irritable bowel syndrome in China: A review.” National Center for Biotechnology Information. Web. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4342906
- “What is IBS?.” About IBS. Web. <http://www.aboutibs.org/what-is-ibs.html